


Skin cancer is rarely lethal, with an extremely high recovery rate when diagnosed early. Even more important, because most types of skin cancer have been linked to long-term sun exposure, you can take steps to reduce the likelihood that you will be diagnosed with skin cancer. In this animation, you will learn not only what skin cancer is and how it develops, but also what you can do to prevent it as well as the treatment options available to those who have been diagnosed.
The cells in your body continuously divide, or proliferate, in order to grow as well as repair or replace damaged cells in the body. Cell division is a highly regulated process. So what regulates these cells? Specific genes, which are coded in your DNA, are responsible for controlling cell division by communicating when to start and stop dividing. If the DNA that makes up these genes is damaged, or mutated, and not repaired properly, the genes may not function correctly. In some cases, DNA damage to a gene that controls cell division may cause a cell to divide uncontrollably. When this happens, a tumor develops. It is important to realize that not all tumors are cancerous. Benign tumors are generally localized to a specific area and do not invade surrounding tissue. In contrast, cancerous tumors invade surrounding tissues and can metastasize, or spread, to other areas of the body.
Now that you have a general idea of what cancer is and what causes it, let’s take a look at how skin cancer develops. Like other types of cancer, skin cancer often starts with DNA damage. DNA damage can be caused by many different carcinogens, but UV radiation from the sun causes most of the damage that eventually leads to skin cancer. Damage that occurs due to occasional sun exposure is usually repaired by built-in DNA repair mechanisms in your body. But, long-term sun exposure can lead to DNA damage that is not repaired. If this damage occurs in genes that are responsible for controlling the division of skin cells, these cells may begin to divide uncontrollably, which can result in skin cancer.

Skin cancer typically affects three different types of cells in the epidermis, known squamous cells, basal cells, and melanocytes. Squamous cells are cells that have flattened as they progress from the basal cell layer toward the skin’s surface, where they are shed. Basal cells are the bottommost epidermal cells that lie along the junction between the epidermis and dermis. As these cells divide, they produce new cells that eventually become squamous cells, which constantly replace the dead skin cells that are shed at the skin’s surface. Melanocytes are a special type of cell located in the basal layer of the epidermis. These cells are responsible for producing melanin, or pigment, which gives your skin and hair its color.

There are often warning signs that can indicate that you are at risk for developing skin cancer. One of these signs is the development of actinic keratosis. Actinic keratosis may be difficult to distinguish from skin cancer, but is typically easily treated if diagnosed early. Most common in people who are forty or older, actinic keratoses are generally caused by long-term exposure to ultraviolet light from the sun. Ultraviolet light damages epidermal skin cells, which causes them to develop abnormal characteristics. While these changes do not cause the cells to become cancerous, they are considered precursors to skin cancer. Much like skin cancer, actinic keratoses generally develop in areas that have been exposed to large amounts of sun such as the face, neck, ears, lips, forearms, and hands. Actinic keratoses appear as rough, callous lesions, and vary in color from light beige tones to dark brown and range in size from a small dot to approximately an inch in diameter.

Accounting for more than eighty percent of diagnosed cases in the United States, basal cell carcinoma is the most common form of skin cancer. Basal cell carcinoma originates in basal cells and typically does not grow very rapidly. Basal cell carcinoma tumors usually grow in a localized area and do not spread to other areas of the body. However, early detection and treatment will prevent the tumor from spreading into surrounding tissue and causing more damage. Scientists believe that this form of cancer is primarily caused by long-term sun exposure; therefore it most commonly occurs on sun-exposed areas such as the face, ears, head, and chest. Basal cell carcinomas can take on a variety of different forms, appearing as shiny bumps, wounds that will not heal, or even red, irritated growths.
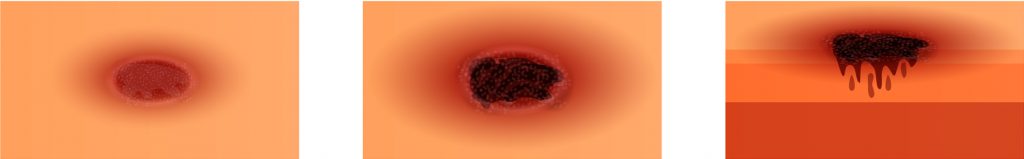
Squamous cell carcinoma is the second most common form of skin cancer in the United States, accounting for less than twenty percent of skin cancer diagnoses. Squamous cell carcinoma originates in squamous cells, and like basal cell carcinoma has been linked to long-term, cumulative sun exposure. This type of cancer is more likely to metastasize, or spread, to other areas of the body through the lymph nodes or bloodstream than basal cell carcinoma, making it more difficult to treat and possibly lethal. However, with early detection, treatments are typically very successful. Like basal cell carcinoma, this form of cancer is most commonly found on sun-exposed areas such as the face, ears, head, and chest. Approximately one inch in diameter, squamous cell carcinoma can look like a red, scaly lesion, wart-like bump, or a wound that does not heal.

Although melanoma accounts for fewer than five percent of the skin cancer diagnoses, it is the most lethal form of skin cancer. However, even this aggressive form of cancer can be treated successfully if diagnosed early. Unlike non-melanoma skin cancers, which are generally linked to the effects of long-term sun exposure, melanoma has been associated with periods of intense sun exposure such as sunburn. In addition, research has shown that certain genetic variants can contribute to melanoma. This form of skin cancer originates in melanocytes and can metastasize, or spread, to other areas of the body, making it more lethal than other types. Melanoma may first appear as a mole on the back, legs, hands, fingers, soles of feet and toes, and the mucous membranes that line the nose and mouth.Step 9: PreventionUltraviolet light plays a critical role in the development of skin cancer, and therefore protecting yourself from the sun is the best preventative step you can take. Avoid unnecessary sun exposure, and protect yourself by covering up with long sleeved shirts, pants, and wide brimmed hats when possible. If your skin will be exposed, dermatologists recommend a SPF 15 or higher sunscreen that protects against both UVA and UVB forms of sunlight.
For the scar free treatment of thin skin cancer and pre-cancerous growths where surgery would be disfiguring
Photo Dynamic Therapy (PDT) for thin skin cancers and pre-cancerous skin growths
Porphyrins are naturally occurring chemicals that when exposed to light glow or burn. This phenomenon has been exploited to successfully treat many different kinds of cancer.
Skin cancers which are confined to the epidermis (upper skin layers) and pre-cancer growths (those that will eventually become skin cancers) can be treated very successfully with PDT. These types of tumours and growths tend to be thin but large. To remove them surgically is complicated and often requires a disfiguring skin graft. Surgery is not always successful because of the tendency of these lesions to form discrete satellite clusters.
PDT is a recognised treatment for:-
How does PDT work?
The porphyrin chemical is absorbed by abnormal cells only. Natural light is shone onto the skin either at a high dose over a short time or at a low dose over a longer time period. Two treatments are required separated by at least two weeks.
How is the treatment carried out?
You will be asked to attend the clinic a minimum of 3 hours before hand. At this time the porphyrin containing cream will be applied to the skin to be treated and then covered. After 3 hours, the cream is wiped off and natural light is shone onto the skin with either a halogen light source (approx 9 mins) or an IPL device (approx 1 min).
Am I suitable for treatment?
There are no contra-indications except pregnancy and a few rare skin and liver disorders. If a scar free result is important to you, then you should seriously consider PDT.
Is it safe?
The treatment is uncomfortable when the light is being shone onto the skin. The skin will have the appearance of a graze or sunburn after treatment and slowly settle back to a normal flesh colour. Any blotchiness or freckles will also be removed from the treated area.
How many treatments are necessary?
Two – one treatment each week.
Aftercare
Avoid sun exposure on the treated area and keep it dry for 24hrs.
